Behind every great tooth is a healthy gum. In our pursuits of bright and perfectly aligned teeth, we can easily overlook the impact that gums have. Gums attach to the teeth and form a seal that protects them and the underlying bone.
Healthy gums typically appear pink in color, feel flat to the touch, and do not cause soreness or pain. X-ray and examination results will reveal a firm and dense supporting bone. As long as you maintain proper dental hygiene at home, and receive regular dental cleanings and checkups, your gums are likely to remain healthy.
Gum disease ranges from a mild to serious infection that usually results from improper hygiene. It damages the soft tissue of the gums and the bones that hold the teeth in place. Gum disease is the leading cause of tooth loss, and it occurs in four stages: gingivitis, early periodontitis, moderate periodontitis and advanced periodontitis. Each stage is progressive and poses an increased risk to your gums, teeth, and surrounding bones.
Risk Factors for Gum Disease
In addition to poor hygiene, smoking is the second most significant risk factor for gum disease. Smoking also can make treatment for gum disease less successful. Other risk factors include diabetes, hormonal changes in girls and women, illnesses that interfere with the immune system, medications that cause dry mouth, and genetic susceptibility.
Patients with crowding of the teeth are at a higher risk for gum disease than those with adequate spacing because crowding makes it difficult to brush and floss teeth correctly. For the same reason, wearing braces also increases your risk of developing gingivitis, the early stage of gum disease. It is important to follow your orthodontist’s instructions for vigilant oral care while you are in orthodontic treatment.
Gingivitis
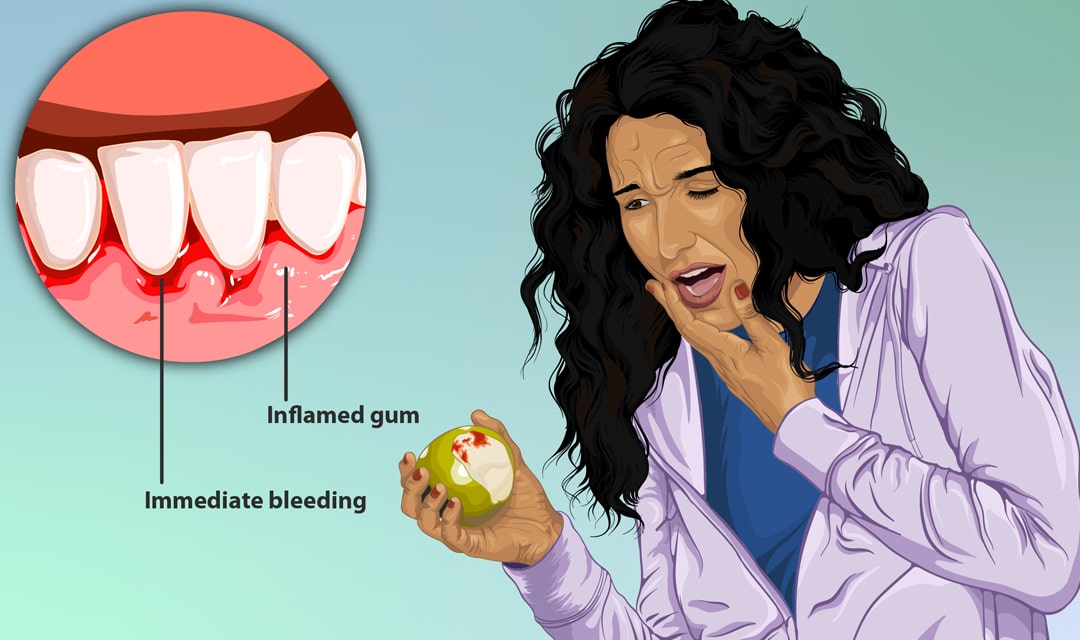
Gingivitis is inflammation caused by plaque (the buildup of harmful bacteria and debris) that forms on and around your teeth. Bleeding during brushing or flossing is often the hallmark indicator of this condition. Swelling may also cause slightly reddened and puffy gums. Some patients experience irritation or soreness, but many do not feel discomfort. Because gingivitis can be completely painless, watching out for its visual signs is key to early detection and treatment.
Never ignore gingivitis, as it is the only stage of gum disease that is completely reversible. Once it progresses into the phases of periodontitis, the damage to the gums, teeth and bone will be permanent. The remedy for gingivitis is better hygiene. Brush at least twice per day with fluoride toothpaste, floss daily to remove plaque from between the teeth, and rinse with an antibacterial mouthwash. Rinsing with salt water also can reduce swelling. The gums should return to normal within two weeks of regimented care. Regular cleanings and checkups are important preventative measures for gingivitis, so make sure you are on schedule with those routine appointments.
Early Periodontitis
Early periodontitisoccurs when infection in the gums spreads to the fibers and bones supporting the teeth. Early periodontitis can be managed but not cured. According to the American Dental Association, more than 47 percent of adults older than 30 in the United States suffer from chronic periodontitis.
In this stage of gum disease, bacteria multiply faster and become more aggressive, often resulting in minor bone loss. The gums detach as they become more inflamed, creating small gaps, or pockets, about four to five millimeters deep (a healthy mouth has pockets that are one to three millimeters). These pockets are highly susceptible to further infection. The gums will take on a deeper shade of red, and you might detect a slight odor. To manage this stage of gum disease, you will need to establish and stick to a proper hygiene routine.
Scheduling a deep cleaning at your dentist’s office also might be necessary to remove deposits of bacteria that are deeply rooted in your gums. Using a technique called scaling and root planing, the dentist can reach deep enough to clean the pockets. Scaling removes plaque and tartar that have accumulated below the gums, while planing smoothes the roots to help the gums reattach to the teeth.
Moderate Periodontitis
Moderate periodontitis can involve significant gum and bone damage. At this point, bacteria has seeped into the pockets around the teeth and caused them to deepen to about six or seven millimeters. Bacteria continue to attack and dissolve the bones, but now they move into the bloodstream as well, triggering an inflammatory response throughout your body. A noticeable odor often is detectable. Gum recession often occurs at this stage, causing the teeth to appear longer. The gums will become red, swollen and tender, and you might begin experiencing tooth sensitivity and pain while chewing. Perhaps the most disturbing symptom of moderate periodontitis is the loosening of the teeth caused by bone loss.
Like early periodontitis, this stage is irreversible and will require significant effort to treat and maintain. Scaling and planing are used and might need to extend over several sessions. Topical or oral antibiotics may be needed to control the infection. Because the condition is permanent, your dentist will probably ask you to return more frequently for routine cleanings and checkups.
Advanced Periodontitis
Advanced periodontitis is the most severe form of gum disease you can have. At this stage, the pockets around the teeth have reached eight millimeters or deeper, and bacteria continue to aggressively attack your bones, bloodstream and immune system. You likely will have a bad taste and strong odor coming from your mouth, and pus may begin to ooze from the gums. The risk of bone loss with advanced periodontitis is as high as 90 percent, so the teeth will continue to loosen and may fall out or require extraction. Pain will increase, especially while chewing.
However, this stage of gum disease is more than just a dental problem. Advanced periodontitis has been linked to a host of serious medical conditions, including heart disease, dementia, stroke, diabetes, rheumatoid arthritis, and respiratory diseases. Additionally, an infection in your bloodstream could become life-threatening if it is acute.
This severe stage of gum disease requires surgical intervention. Flap surgery reduces pocket sizes around the teeth by using small incisions to peel back the gums to deep clean. The surgeon then fits the gums snuggly around the tooth to reduce the size of the pocket. The underlying bone also may need to be recontoured. A bone graft uses fragments of your own bone, donated bone or synthetic bone to replace what gum disease has destroyed. A soft tissue graft will replace some of the receded gum with tissue from your mouth or a donor. Guided tissue regeneration uses an artificial membrane to keep soft tissue from growing into the gaps and to allow the regrowth of bone that was destroyed by bacteria. You may require one or more of these procedures, as well as others.
If left untreated, gum disease can cause serious health problems. It’s best to adopt a rigorous dental hygiene regimen and catch any signs of gingivitis before the disease progresses. If you are concerned about gum disease or wonder how it may affect your orthodontic treatment, schedule a complimentary consult with one of our board-certified orthodontists today.